Suicide ideation and behaviour of older people in care homes: Who is giving up?
Moving into a care home is a major life event in later life and most people will need a lot of support to adjust as well as be able to deal with the many losses that may have led them to living in institutional care. For some this can contribute to, or escalate depression and result in suicide ideations and behaviours in the form of self-neglect and self-harm. Trish Hafford-Letchfield reports.
There are generally much fewer studies on suicide in later life than for other populations. As baby boomers are a group with historically higher rates of suicide, we can anticipate that will need to have suitable strategies for suicide prevention as they reach later life (Conwell et al, 2011).
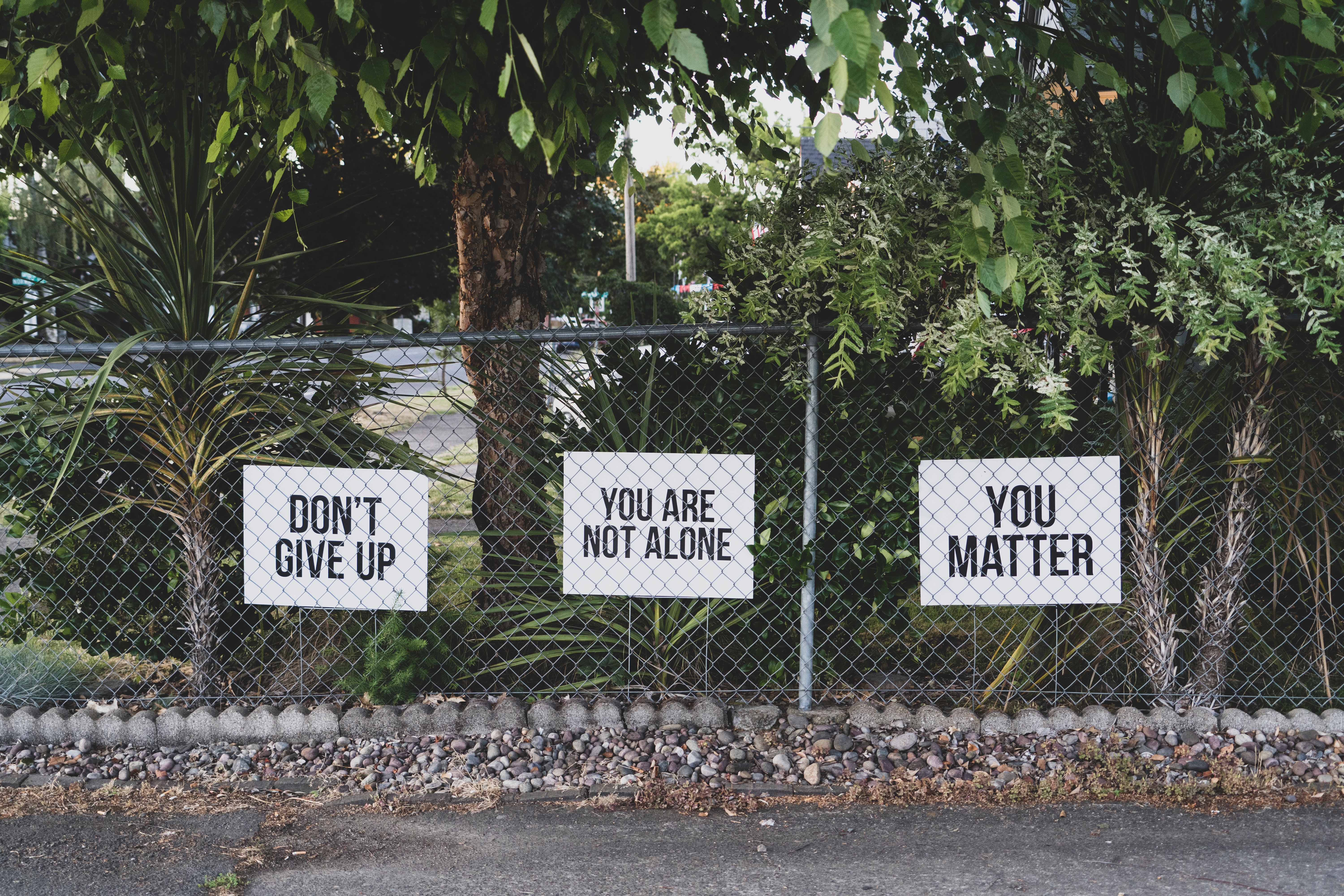
Suicide prevention strategies however tend not to prioritise older people and this particularly includes reaching out to people living in care homes where suicide is hardly recognized, understood or documented (Murphy et al, 2018). Care homes are a significant place of care until death so why do we tend to treat or see people’s end of lives differently? (Age UK, 2013).
Suicidal ideation and behaviour of older people living in care homes is often referred to as ‘giving up’ or ‘turning to the wall’ and we found that this was not an uncommon experience in our exploratory study of care home staff’s experiences of this phenomena (Hafford-Letchfield et al, 2018).
Individuals would often stop eating, drinking, refuse care and express the wish to die.
Trish Hafford-Letchfield
While responding to these situations requires observations and capabilities of care staff in daily contact with people ‘giving up’, we observe that staff were also given the least support and were less likely to be involved in any interventions that followed.
There is very little known from the perspective of older people themselves about what situations might lead to them giving up and what they want to happen, who can support them and how: why not to ask them directly about their thoughts of self-harm and hopelessness? how to alleviate things that are stressing them? how to facilitate relationships within which they can confide? We also found little consistency in the literature about what can help to address the suicidal ideation and behaviour of people living in care homes and the type and quality of interventions needed including those which engage with end-of-life care (Gleeson et al, 2018).
Suicide in later life is a complex and multi-faceted issue where ageing, particularly within marginalised groups needs to be included. Involving older people themselves in these debates, conducting research and designing and evaluating suicide prevention is another step towards combating ageism and mental health.
Read also:
Promoting inclusive care environments for older people with sexual and gender diversities
‘Bring back that loving feeling’: Sexuality in later life and the impact of ageism
—
Trish Hafford-Letchfield is Professor of Social Work at the University of Strathclyde, UK. She is a qualified nurse, social worker and educator and her main interests are in promoting the quality of older people from marginalised communities.


Facebook Comments