How is ageism linked to inappropriate medication use in older patients?
Jovana Brkic and Daniela Fialova explain that ageism affects the way medicines are prescribed and managed, often leading to negative effects for older patients
As people get older they have more difficulties with recovering from minor injuries, are more likely to develop more medical conditions and consequently use more medications. We do not have enough information about how appropriate certain medications are for older people and therefore medication treatment plans in older adults are not yet adequately individualized.
Older people are generally underrepresented in clinical trials, clinical guidelines are more focused on single diseases and are mostly based on results of trials on healthier younger population.
Older persons are also usually not involved in decision making about their medical treatment and interventions are many times focused on “cure” than on older patients’ quality of life and preferences. For many older patients improvement of quality of life, such as being able to pursue usual activities and being free of pain is the highest priority.
Many healthcare workers are not adequately educated in the field of geriatrics and geriatric pharmacotherapy, although older persons are the most frequently represented patient group in different health care settings and the most common users of medicines.
Polypharmacy, i.e. the concurrent use of multiple medications and inappropriate prescribing, is more prevalent in the older population than other age groups, even if a lot of tools now support better prescribing practices in older patients. Polypharmacy puts older patients at risk of negative health outcomes, unnecessary hospitalisation but also creates additional expenses for individuals and health care systems.
In order to minimise ageism in health care and improve older patients’ treatment, several strategies should be implemented, particularly:
(1) the number of older persons in clinical trials should increase to have more evidence about the real efficacy and safety of medications in the older age group;
(2) existing clinical guidelines should incorporate more information on older adults;
(3) healthcare professionals should be more educated in geriatric pharmacotherapy and individualized, person-centered approach; and
(4) the emphasis must be given on shared decision making and empowerment of older persons to influence the appropriate choice of their medications.
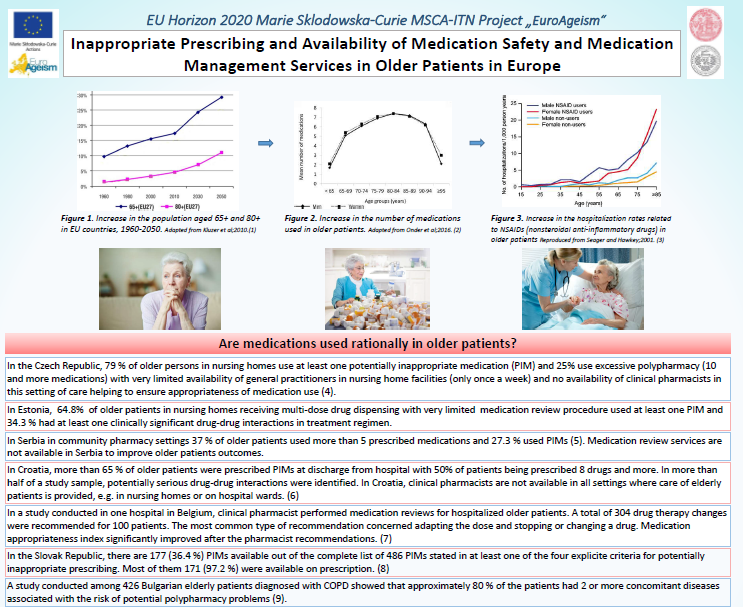
See the full poster “Inappropriate Prescribing and Availability of Medication Safety and Medication Management Services in Older Patients in Europe” using the link below:
For more information:
- Book Chapter Ageism and Medication Use in Older patients:
https://link.springer.com/chapter/10.1007/978-3-319-73820-8_14 - EUROAGEISM H2020 project, FIP7 program webpage:
https://portal.faf.cuni.cz/Projects/Euroageism-Project/
—
This research is part of the EuroAgeism project, which has received sponsorship from the Marie Skłodowska-Curie EU Framework for Research and Innovation Horizon 2020 Program under Grant Agreement No. 764632, Horizon 2020-MSCA-ITN (2017-2021). Authors of the article and project responsible persons:
- Jovana Brkic, MSc
Main ESR in FIP7 program of the EUROAGEISM H2020 project
Department of Clinical and Social Pharmacy, Faculty of Pharmacy, Charles University, Czechia - Daniela Fialova, PhD, PharmD, BCCP
Chair of the EUROAGEISM H2020 project-FIP7 program
Head of the University Educational Centre in Clinical Pharmacy, Faculty of Pharmacy, Charles University
Photo by rawpixel initially downloaded on Unsplash.org


Facebook Comments